New longitudinal study examines how early childhood adversity can increase risk of adolescent substance use
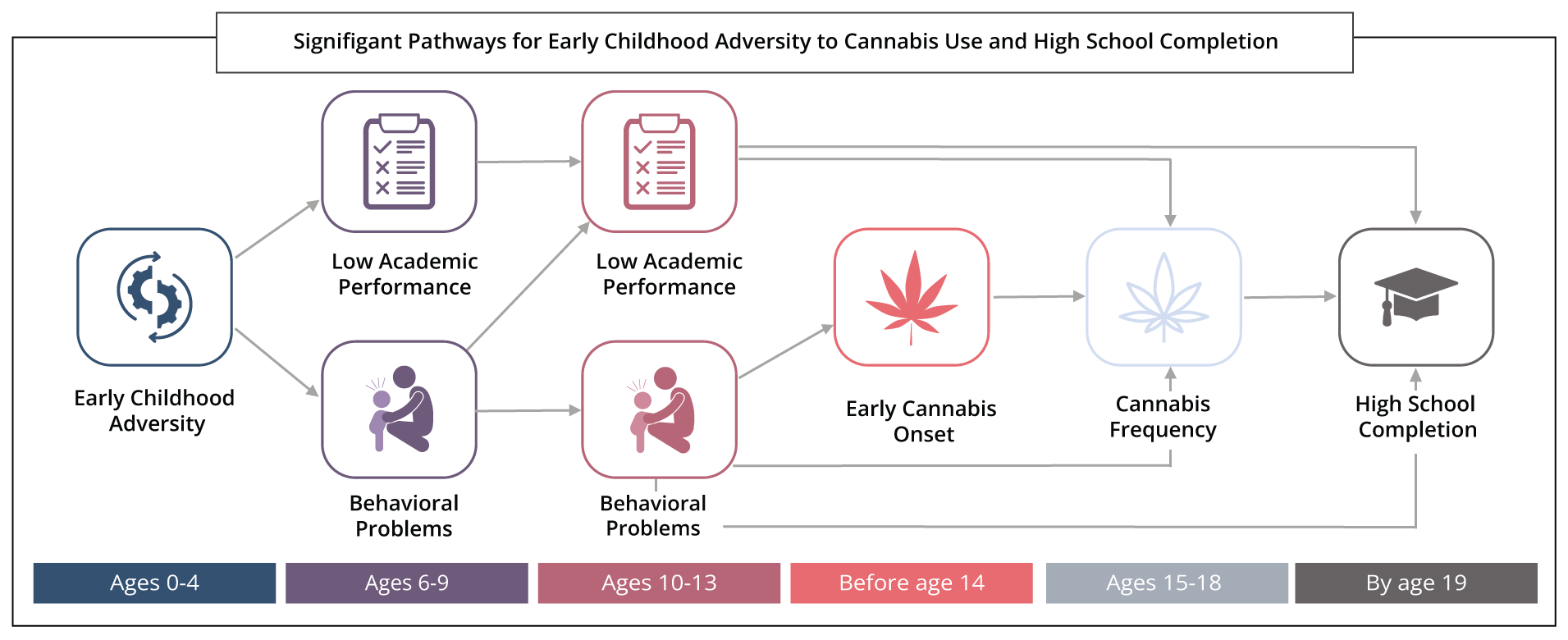
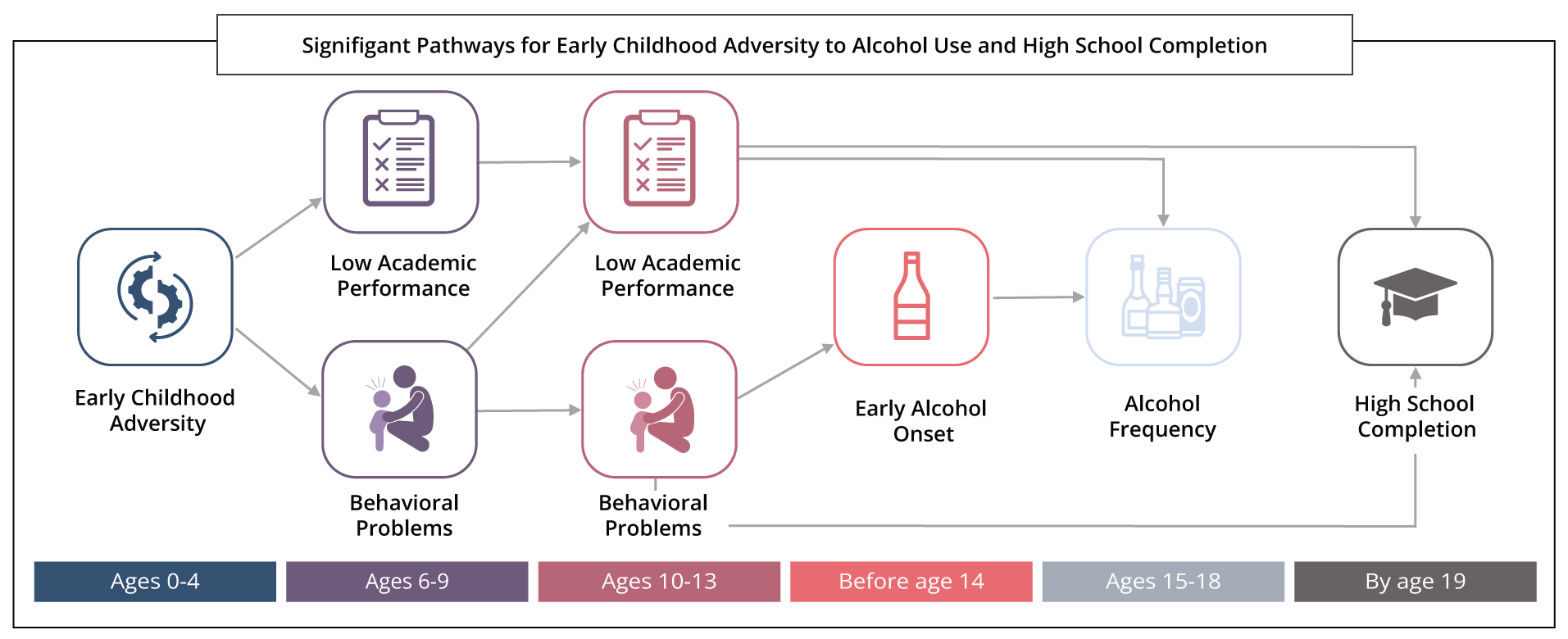
A new study published in the journal Drug and Alcohol Dependence found pathways linking early childhood adversity (ECA) before the age of five and alcohol and cannabis use in adolescence. ECA was associated with both greater behavioral issues and lower academic performance in childhood, which predicted increased substance use in adolescence and, in turn, lower high school completion by age 19, according to the research team at the Alcohol Research Group (ARG), a program of the Public Health Institute.
Exposure to adverse conditions early in life can affect a young child’s neural, cognitive, and emotional development. Extensive research has established a strong association between childhood adversity before age eighteen and substance use in adolescence and adulthood. However, little attention has been placed on early life adversity and the mechanisms linking this with outcomes many years later.
“Early childhood is a particularly sensitive period in one’s life, and it is crucial to better understand their underlying associations and pathways that can elevate the risk for later life substance use,” said Scientist and lead author Camillia Lui.
The research team leveraged existing data from a large cohort of US children to analyze ECA before age five using a cumulative score of four indicators — maternal heavy drinking/drug use, low emotional support, low cognitive stimulation, and household poverty.
By analyzing alcohol and cannabis separately, researchers found some similarities and differences in pathways. For example, ECA increased the frequency of use for both substances at ages 15 to 18 through intermediary factors such as externalizing and internalizing problems during middle childhood (ages 6–9) and again in early adolescence (ages 10–13). ECA was more consequential for adolescent cannabis use than alcohol.
Results differed for the two substances when examining the pathways to early onset of substance use before age 14. Findings showed that ECA had direct effects on early cannabis onset, but the same was not found for early alcohol onset.
“We had expected ECA to equally affect early alcohol and cannabis use, but it was primarily cannabis use. This finding may be influenced by declining alcohol consumption and steady increases in cannabis use in adolescence, increased cannabis legalization in the US, and more favorable attitudes toward cannabis,” Lui added.
In other findings, ECA also had more immediate impacts on academic problems in childhood. However, it was ECA’s effect on behavioral issues which increased adolescent cannabis use and lowered high school completion by age 19. Moreover, a direct path linking ECA and lowered high school completion remained, suggesting other factors not captured in this study are relevant.
The study team calls for greater attention to early-to-middle childhood as an opportune time to mitigate the effects of early childhood adversity.
“Experiencing early childhood adversity does not predetermine specific behaviors in childhood, adolescence or adulthood. However, the better we are able to identify the pathways linking adverse exposures before the age of five to substance use, the better we can set support systems in place to make children less susceptible to adverse outcomes later in life,” Lui said. “Based on study findings, interventions that can address ECA and early behavioral problems can help to disrupt pathways leading to greater adolescent cannabis and alcohol use and help improve educational outcomes.”
Researchers used prospective data from the National Longitudinal Survey of Youth 1979-Child/Young Adult Cohort, an intergenerational study of mothers and their children. This analysis focused on children born 1984–1999 and followed through 2016 (n = 5521).
The study “Associations between early childhood adversity and behavioral, substance use, and academic outcomes in childhood through adolescence in a U.S. longitudinal cohort” by Camillia K. Lui, Jane Witbrodt, Libo Li, Christina C. Tam, Edwina Williams, Zihe Guo, and Nina Mulia is available at: https://doi.org/10.1016/j.drugalcdep.2023.109795.
~
Support for this paper was provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) under award number R01AA026956 (N. Mulia, PI) at the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.